During summer, there will be countless opportunities to go for a swim in pools, lakes, rivers, the sea, and even water parks.
But if you, or your child, are living type 1 diabetes (T1D), this fun activity can raise questions, or even cause anxiety, which is why preparation is key.
What impact can swimming have on blood sugar? Will the sensor of your continuous glucose monitor (CGM) fall off? Can you even go swimming with an insulin pump?
Here’s what you need to know about swimming and T1D.
Blood sugar management
The impact of your swim on your blood sugar levels will depend on the water activity in question.
You (or your child) could use this time in the water to:
- Do swimming laps. In that case, blood sugar levels could decrease, just like with any other low- to moderate-intensity exercise. When swimming in the sea, the waves can increase the intensity of the swim as well as your risk of low blood sugar. Conversely, your blood sugar could increase if you do activities such as interval-based swimming laps or water polo.
- Relax or go for a leisurely swim. In that case, the risk that your swim will impact your blood sugar is low.
However, the heat can also play a role and lower blood sugar levels. So, you need to be extra cautious in very high temperatures.
If it’s your first swim with T1D, the stress of the new environment (water, waves) can sometimes increase blood sugar levels.
To properly assess the impact of swimming on blood sugar, the best solution remains to regularly check your levels before, during and after. Planning the activity can also help you to implement strategies to limit its impact on blood sugar and avoid hypoglycemia.
For example, keeping a physical activity log where you write as much information as possible (e.g., blood sugar measurements, insulin doses, type of activity based on time of day) can be a good way to assess the strategies that you test out.
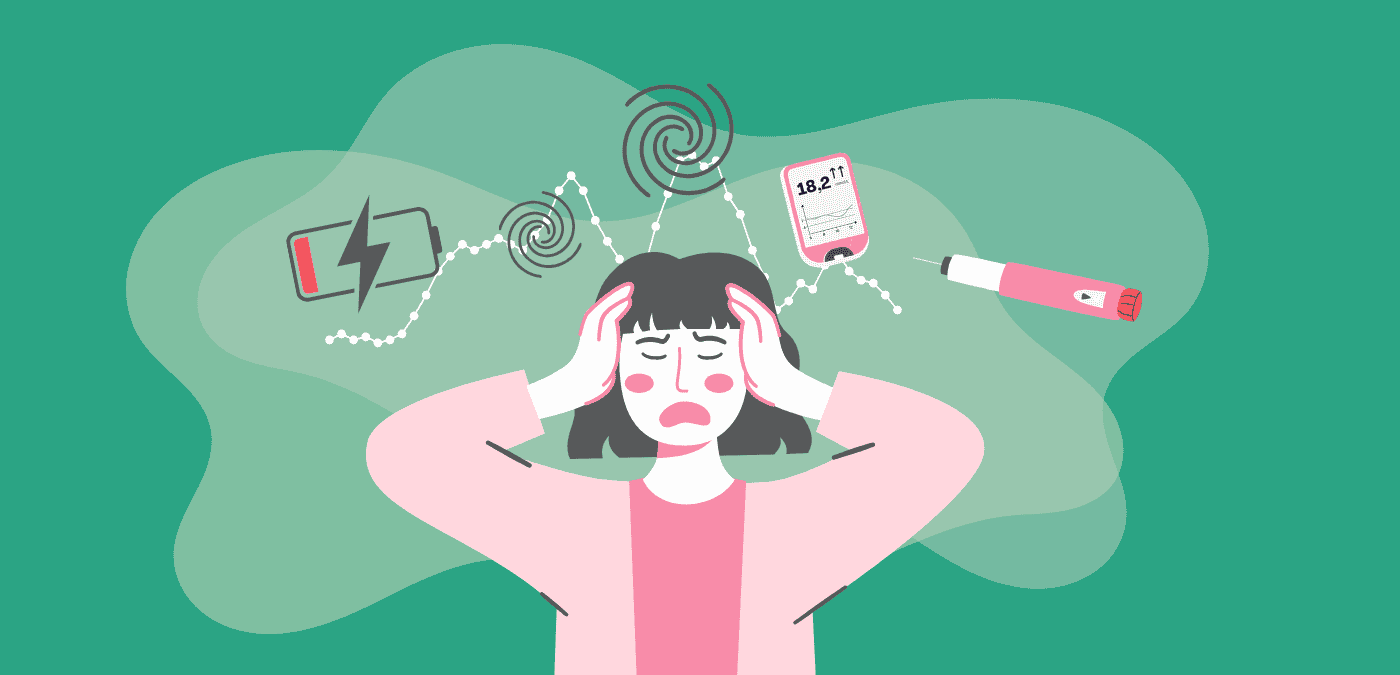
Continuous glucose monitors
If you or your child use a CGM (e.g., Dexcom, FreeStyle Libre), the sensor applied to the skin (and its transmitter, if applicable) can go in the water and stay in place during your swim. However, it’s possible for the device to fall off. To avoid this kind of problem, you can secure the sensor by using certain adhesive products under or over it, or bands. Note that applying a dressing over the Dexcom transmitter is not recommended (it must be apply around it) because this could lead to a loss of signal.
In the case of monitors that automatically transmit data (e.g., Dexcom, Guardian) and/or provide alerts (e.g., FreeStyle Libre 2), the water itself or the distance from the receiver/cell phone can hinder data transmission. This loss of communication can prevent your CGM from displaying your blood sugar levels and triggering alerts.
Insulin pumps
If you or your child use an insulin pump, the watertightness of the device varies according to the manufacturer.
-
Pump with tubing (e.g., Medtronic, Tandem).
Even when manufacturers say their pumps are waterproof, this very much depends on the condition of the pump (e.g., age, seal watertightness). In general, these companies will easily and quickly replace a pump in the event of problems, but having a non-working pump can be an extremely stressful situation. That’s why these pumps are considered more to be water-resistant (e.g., accidental fall in the water, drop of water on the pump). However, there are two strategies you can use to enjoy some water fun and preserve your peace of mind:
-
-
- Disconnecting the pump. This is the most recommended strategy. The catheter stays in place, but you remove the tubing and the pump (in theory, a cap needs to be placed at the end of the removed tubing for hygiene reasons). It is suggested not to disconnect the pump for more than two hours and to regularly check blood sugar (before/during/after). And don’t forget to reconnect the pump adn reactivate insulin once your swim is over!
- Using a waterproof case. There are specially designed cases that can go in the water and keep their contents dry (e.g., Aquapac). These cases can also help to avoid sand coming into contact with the pump. Waterproof cases are currently being developed (e.g., Diassentials)
-
-
Pump without tubing.
The pod (an insulin-containing wireless device that is applied to the skin) that is used with the Omnipod pump is waterproof. However, you need to make sure that the pod is securely in place. There are products that help the device stick to the skin, and also dressings that can be applied over the pod.
Since the pod contains insulin, you need to be cautious when swimming in very warm or very cold waters (e.g., spas), which could impact insulin efficacy. Don’t forget to change pods if you have any doubts.
Emergency kit
One thing cannot be overstressed: preparing is key for being able to face any possible situation.
In addition to carrying your blood sugar meter (capillary meter or CGM) and your insulin pens or pump, don’t forget to:
- Bring some sugar (in case of hypoglycemia) and snacks.
- Keep your insulin in a cool shaded place (especially in high heat). There are cases that can keep your insulin cool (e.g., FRIO, Glucology). If you’re unsure about its efficacy, change the insulin inside your pen or pump.
- Bring the necessary supplies to change your CGM’s sensor and/or your pump’s catheter (or pod) in case it falls out.
- Stay hydrated. The heat can lead to dehydration and can increase blood sugar.
- Bring some sunscreen. This basic tip is important for avoiding sunburns, which can lead to blood sugar spikes due to the stress on the body.
Now, it is time to enjoy the water safely!
(First published in 2022; updated in 2024.)